Study design
There were 1462 infertile patients (one year of unprotected intercourses without pregnancy in a couple without detected female infertility factors); Ages ranged from 22 to 43 years, with a mean age of 31.6 ± 3.2 years who visited at the male department and reproductive Medicine Center at Women’s Hospital of Nanjing Medical University between August 2018 and September 2019 were included in the present study. The inclusion criteria are: (1) Sperm malformation rate ≤ 96%; (2) The female was ≤ 40 years old, body mass index (BMI) ≤ 30 kg/m2, and corresponding (blood routine, urine routine, reproductive hormone, serum anti-sperm antibody) tests were at normal levels. The semen test (mycoplasma, chlamydia, gonococcal) was negative. (3) FSH < 10.00 IU/L was detected in the outpatient department of our hospital for the first time. The cause of infertility was only the fallopian tube and the number of eggs obtained was ≥ 514. (4) Both couples received IVF-ET or ICSI for the first time. Exclusion criteria : (1)The male partner had severe oligospermia (sperm concentration of the male partner < 5.00 × 106 /mL). (2)Excluded were those with family diseases, genital trauma, and organic lesions, urological and reproductive diseases (e.g. varicocele, cryptorchidism, prostatitis, epididymitis, leukocytopenia, hematospermia, and azoospermia. (3)Excluded were those with diseases: endometriosis and Polycystic Ovary Syndrome (PCOS) (4) The male who has severe impairments of heart, liver, and kidney function, smokers were excluded.. (5) Female genital malformation such as the double uterus, single horn uterus, mediastinal uterus, severe uterine cavity adhesion, endometrial thin and other conditions affecting embryo implantation. (6) The woman had thyroid disease, diabetes, and other endocrine diseases15. According to DFI levels, there were 468 cases in group I (DFI ≤ 15%), 518 cases in group II (15% < DFI < 30%), and 476 cases in group III (DFI ≥ 30%).
The IVF mainly consisted of couples with female factor infertility, and the criteria for ICSI was a total sperm count of < 800,000 after gradient centrifugation. A total of 101 pairs of IVF-ET/ICSI infertile couples were included in the study (including 56 cases of IVF and 45 cases of ICSI) and subdivided into IVF-I group (DFI ≤ 15%), IVF-II group (15% < DFI < 30%), IVF-III group (DFI ≥ 30%), ICSI-I group (DFI ≤ 15%), ICSI-II group (15% < DFI < 30%) and ICSI-III group (DFI ≥ 30%) according to DFI value.Among the 56 pairs in the IVF group, the male age was 22–43 years old (32.63 ± 5.21), and the female age was 25–40 years old (31.62 ± 4.05). In ICSI group of 45 pairs, the male age ranged from 26 to 51 years old (32.83 ± 5.62), and the female age ranged from 25 to 40 years old (31.63 ± 5.32). The present study was approved by the Ethics Committee of the Women’s Hospital of Nanjing Medical University and was conducted in accordance with the Declaration of Helsinki. An information sheet was provided to all participants. Written informed consent was obtained from all participants. The relevant guidelines and regulations of the local institute were strictly followed when conducting the study. Participants were informed that they could withdraw from the trial without giving a reason.
Semen collection and routine semen analysis
According to the Laboratory Manual of the WHO for the Examination and Processing of Human Semen (5th edition) and WHO Manual for the Standardized Investigation, Diagnosis and Management of the Infertile Male11, semen samples were collected by masturbation after 2 to 5 days of ejaculatory abstinence16. The duration of abstinence was recorded. Each semen sample was directed into a sterile plastic cup and liquefied in an incubator at 37 °C. The semen liquefaction was complete, 10 μL of the sample was taken and counted, and sperm concentration and viability were recorded.
The routine semen analysis was performed with a semen quality detection system (CFT-920, Jiangsu Ruiqi Life Science & Tech Dev. Co.Ltd) with supporting reagents. The main parameters were as follows17. Image acquisition frame: low and middle sperm concentration collected at 20 Hz, and high sperm concentration at 7 Hz; acquisition interval: 3 ms; maximum sperm motile velocity: 200 μm s−1; area range of spermatozoa head detected at 7–60 μm2. Index of sperm motility: straight line velocity (VSL). Grayscale thresholds were set to collect spermatozoa and exclude nonsperm granules. According to the thresholds set for sperm analysis, sperm images were collected and analyzed. The sample was considered normal if semen volume had > 1.5 ml volume, ≥ 15 million/mL sperm concentration, ≥ 40% progressive motility and ≥ 4% normal morphology18.
Sperm morphology assessment
For morphological evaluations, seminal smears were stained with Diff-Quik (MICROPTIC S.L. Co., Barcelona, Spain)19. Approximately 10 μl of sperm was smeared into a thin and homogeneous layer on a clean glass slide and was air-dried at room temperature for at least 10 min. The slides were stained and observed under a brightfield microscope (BH-2; Olympus, Tokyo, Japan) at 1000× magnification. According to WHO guidelines, a sperm with a deformed head, midpiece, or principal piece was counted as SDI (sperm deformity index), which is the number of deformed sperm/number of total sperm. For each semen sample, at least 200 sperms (or the whole sperm if the slide had less than 200 sperm) were counted via a double-blinded method. Then, the percentage of sperm with normal morphology was calculated20.
Semen optimization
After the semen was completely liquefied, the sperm was selected by discontinuous density gradient centrifugation combined with the swimming-up method, as follows.
(1) Discontinuous density gradient centrifugation
Two prepared gradient centrifugation media, one with 80% concentration and another with 40%, were preheated to 37 °C in in the incubator. In a sterile conical centrifuge tube, 1.5 ml of 80% gradient centrifuge medium was pipetted under 1.5 ml of 40% medium, and 2.0 ml semen was slowly added onto the top layer. After centrifugation at 300–400×g for 15 min, remove the supernatant, leaving only about 0.5 ml at the bottom. Then 2 ml Fertilization Medium was added to sperm deposition and thoroughly mixed. After one more centrifugation at 300–400×g for 5 min and removing of the supernatant, sperm deposition was transferred to a Falcon 1006 centrifuge tube containing 0.5 ml Fertilization Medium18.
(2) Sperm swimming-up
The Falcon1006 centrifuge tube was tilted at 30—45 °C degree angle in a 37 °C incubator with 5% CO2 and saturated humidity. The process of sperm swimming-up lasted for half an hour, and then the upper sperm suspension was aspirated into another clean Falcon1006 centrifuge tube for later use18.
DFI (SCD test)
To measure the DNA fragmentation in native and DGC-separated semen, the SCD test was performed using the SpermFunc™ DNAf kit (BRED Life Science, Shenzhen, China). Gelled aliquots of low-melting-point agarose in the kit were provided for semen sample processing in Eppendorf tubes. Eppendorf tubes were placed in a water bath at 80 °C for 20 min to melt the agarose and then transferred to a water bath at 37 °C for 5 min for temperature equilibration. A total of 60 μl of sampled semen was added to and mixed with the agarose in the Eppendorf tubes. Then, 30 μl of the semen-agarose mixture was pipetted onto precoated slides in the kit that were covered with a 22 × 22-mm coverslip. The slides were placed on a cold plate in the refrigerator (4 °C) for 5 min, allowing the agarose to produce microgel in which the sperm cells were embedded. The coverslips were gently removed, and the slides were immediately immersed horizontally in solution A and incubated for 7 min. Next, the slides were horizontally immersed in solution B for 25 min. After being washed for 5 min in a tray with abundant distilled water, the slides were dehydrated in gradient concentrations of ethanol (70%, 90%, 100%; respectively) for 2 min, air-dried, and stored at room temperature in opaque closed boxes21.
For bright-field microscopy, the slides were horizontally covered with a mixture of Wright’s staining solution (BRED Life Science, Shenzhen, China) and phosphate buffer solution (BRED Life Science, Shenzhen, China) (1:2) for 15 min with continuous airflow. Then, the slides were washed in running water for 10 s and allowed to dry. Intense staining was recommended to allow the periphery of the dispersed DNA loop halos to be more visible. A minimum of 500 sperm were counted on each sample under the 100× magnification22.
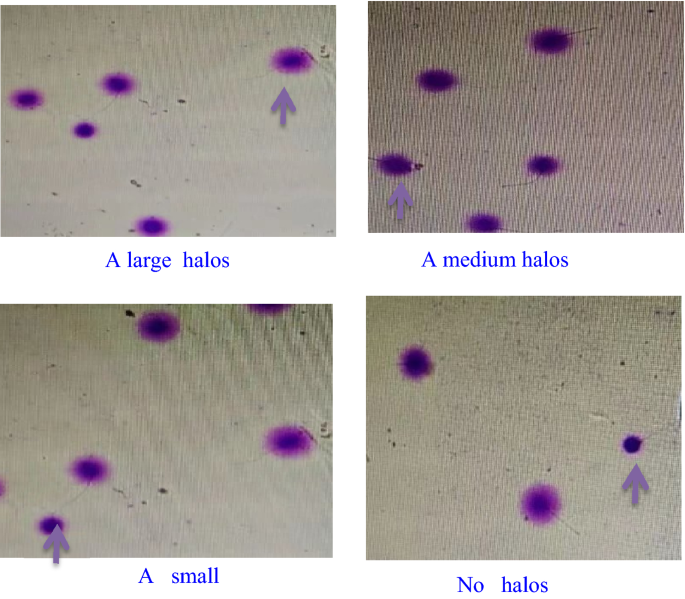
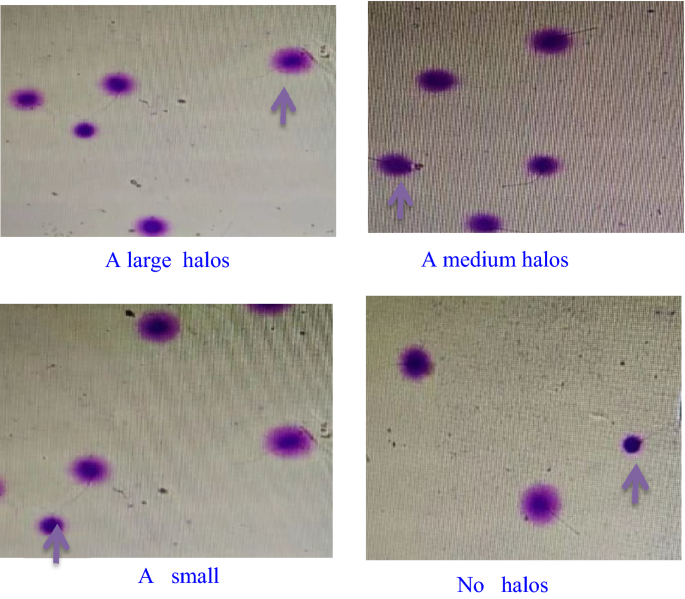
Normal spermatic DNA presented radiate halos, and damaged spermatic DNA presented no or small halos. Fragmented sperm refers to those having a small or no halo (Fig. 1). The thickness of the halo on one side was less than the 1/3 diameter of the head’s thinnest part23. The rate of SDF (%) = the number of sperm with fragmented DNA/the totalnumber of sperm × 100%, and < 25% was considered normal.
Quantitative detection of seminal plasma biochemical indexes
Spectrophotometry was used to test TAC (U/L) and MDA (nmol/mL) levels. MDA levels were determined using the thiobarbituric acid (TBA) method. Semen samples were centrifuged at 4 °C for 15 min with a speed of 2000 r/min. The supernatant was mixed with the reagents supplied in an MDA Assay Kit (Nanjing Jiancheng Bioengineering Corporation, China, A003-2) and incubated at 95 °C for 40 min. Having been cooled at room temperature, the mixture was centrifuged at 4000g for 10 min. The absorbance of the supernatant was measured at 530 nm. All operations were performed according to the manufacturer’s instructions. The MDA concentrations were expressed as nmol/mL24.
Treatment of IVF-ET and ICSI
The woman followed a regular long regimen of gonadotropin-releasing hormone agonist (GnRH-α). The follicle development was monitored by vaginal B-ultrasound and serum estradiol (E2) level. After follicle maturation, human chorionic gonadotropin (HCG) was injected intravascularly. Egg extraction was performed 36 h later under the guidance of B-ultrasound. Fertilization was observed 16–18 h after insemination. Blastocysts were rated by the Gardner method, and D5 score ≥ 3BB or D6 score ≥ 4BB were defined as high-quality embryos. One to two high-quality embryos were frozen and thawed for transplantation, and luteal support was performed after transplantation. 35 days after transplantation, b-mode ultrasonography showed that the primary heart tube beating of the gestational sac was clinical pregnancy25.
Oocyte fertilization and embryo culture and transfer
For IVF fertilization, fresh semen was subjected to DCG in sperm-grade 40% and 80% solutions for pretreatment, followed by the sperm swim-up technique to adjust to a final sperm density of 1 × 106/ml. The solution was then cultured with oocytes for fertilization. In ICSI fertilization, after DCG of the sperm from fresh semen, viable sperm with good morphology were collected under the microscope and directly injected into the egg cytoplasm for fertilization26. The pronuclei of the oocytes were examined 16–18 h after injection to assess the success of fertilization27.
Calculation of IVF/ICSI clinical outcomes
$$\begin{gathered} {\text{IVF\, fertilization\, rate }} = {\text{ the \,number\, of \,fertilized \,eggs\,}}/{\text{\,total \,number\, of\, obtained \,eggs}} \times {1}00\% . \hfill \\ {\text{Fertilization\, rate\, of \,ICSI }} = {\text{number\, of \,fertilized\, eggs\,}}/{\text{number\, of\, M\,}} {\text{II eggs}} \times {1}00\% . \hfill \\ {\text{Cleavage \,rate }} = {\text{the \,number\, of \,fertilized\, cleavage\, embryos}}/{\text{number \,of \,fertilized\, eggs}} \times {1}00\% . \hfill \\ {\text{High-quality\, embryos\, rate }} = {\text{the \,number \,of\, high-quality\, embryos\,}}/{\text{\,number\, of\, normally\, fertilized \,embryos }} \,\times \,{1}00\% . \hfill \\ {\text{Clinical\, pregnancy\, rate }} = {\text{ the\, number\, of \,clinical\, pregnancy\, cycles }}/{\text{\,the \,number \,of\, all\, transplant\, cycles}} \times {1}00\% . \hfill \\ \end{gathered}$$
Statistical analysis
Statistical analyses were performed by with SPSS software Version 22.0 (SPSS Inc., Chicago, IL, USA) for Windows. The measurement data were tested for normality and homogeneity of variance. Data that do not conform to normal distribution and homogeneity of variance will be represented by median (P25, P75). Kruskal–wallis H test was used for comparison between groups, the Nemenyi test was used for pial comparison, and Spearman’s test was used for correlation analysis. Data consistent with normal distribution and homogeneity of variance were expressed by mean ± standard deviation. Comparison between groups was performed by one-way ANOVA, SNK-q test was used for pairwise comparison. Counting data were presented as cases or cases (%), and comparison between groups was performed by χ2 test, P < 0.05 was considered statistically significant.